ASSOCIATION OF PROFESSORS OF GYNECOLOGY AND OBSTETRICS

Cervical Cytology
- Back to Module Listing
- Description
- Learning Outcomes
- Best Practices
- Checklist
- Performance Assessment
- Practical Tips
- Resources
Description
The American Cancer Society (ACS), the American Society for Colposcopy and Cervical Pathology (ASCCP) and the American Society for Clinical Pathology (ASCP) have released new guidelines (2012) for the prevention and early detection of cervical cancer. The guidelines generally advise a reduction in the number of tests women get over their lifetime to better ensure that they receive the benefits of testing while minimizing the harms, and include a preference for co-testing using the Pap test and HPV test for women age ages 30 to 65. The New ACS-ASCCP-ASCP Cervical Cancer Screening Guidelines article may be accessed through the Journal of Lower Genital Tract Disease.
The ASCCP recommends PAP screening to begin at age 21 irrespective of age of sexual onset. Between the ages of 21 and 29, cytology alone is recommended to occur every three years and HPV testing “should not be used to screen.” HPV testing should not be a component of co-testing nor used as a primary standalone screening test. For women age 30-64, cytology and HPV co-testing every five years is preferred but cytology alone every three years is acceptable. PAP screening is recommended to stop at age 65 for women with adequate negative prior screening and no history of CIN 2 or worse, within the last 20 years. “Adequate negative” equals three consecutive negative PAPs or two (2) consecutive negative HPV tests. For women over 65 and “adequate negative” prior screening, PAP screening should not resume for any reason, even if a new partner is reported. Screening after age 65 should not stop if there is any prior history of AIS, CIN 3 or CIN 2. Screening should continue for at least 20 years in all women with a history of AIS, CIN 3 or CIN 2, even if it extends past age 65. No screening is recommended for women who have undergone a hysterectomy, provided the cervix was completely removed and in women without a history of CIN 2 or a more severe diagnosis in the past 20 years.
The learner should:
- Introduce themself to the patient, confirm the patient’s identity and establish how they want to be addressed
- Wash hands (or use an alcohol-based antiseptic) and put on non-latex gloves (if these are not available, an inquiry about latex allergy is necessary before proceeding)
- Explain the purpose of the examination and general steps before beginning
- If this is the patient’s first examination, the student should explain thoroughly and show the speculum and cervical cytology collection devices to the patient
- Drape patient appropriately
- Be sensitive to patient discomfort throughout the examination and provide opportunities for the patient to ask questions
Cervical Cytology Collection
The learner should:
- Select the appropriately sized speculum, warm speculum and test speculum on patient’s leg for comfortable temperature
- Inform patient prior to speculum insertion
- Insert speculum at 45-degree downward angle, then rotate and open when completely inserted
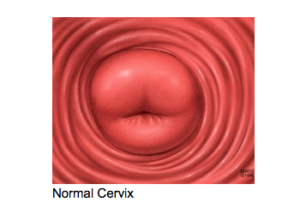
- Visualize the cervix by adjusting the speculum anteriorly or posteriorly
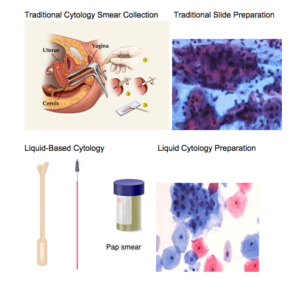
Traditional Slide Cytology Collection
The learner should:
- Use the spatula clover leaf end to collect ectocervical cells or spatula end for vaginal cuff cells, and then smear them in a thin layer on the slide
- On the same slide, smear endocervical cells collected using a cytobrush (only insert cytobrush superficially in pregnancy)
- The student or assistant should spray the slide with cytology fixative immediately after cytology collection and place it in the appropriate container
- The learner or assistant should label the container appropriately
Liquid-Based Cytology Collection:
- Learner should first use the plastic (not wood) spatula to collect ectocervical cells (rotate 360 degrees), then brush-like device (rotate 180 degrees) to collect endocervical cells (only insert brush superficially in pregnancy)
- Both spatula and brush should be swept around the inside of the liquid-based cytology specimen collection container 10 times to loosen the maximum number of cervical cells into solution
- The learner or assistant should label the container appropriately
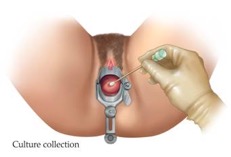
Cervical/Vaginal Culture Collection
The learner should:
- Select appropriately sized speculum, warm speculum and test speculum on the patient’s leg for comfortable temperature
- Inform patient prior to speculum insertion
- Insert speculum at 45-degree angle then rotate and open when completely inserted
- Visualize the cervix by adjusting the speculum anteriorly or posteriorly
- Use the appropriate collection vial with the correct attached swab for each culture
- For Chlamydia and Gonorrhea cervical “cultures,” insert the swab into the endocervix for approximately 10 seconds (insert only superficially in pregnancy)
- For vaginal cultures, obtain a specimen from the posterior fornix
- Insert the swab into the vial, break off the excess swab and cap off the collection vial/tube securely and label the specimen
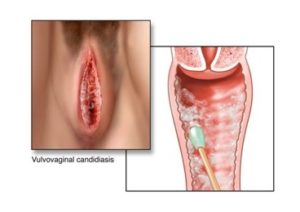
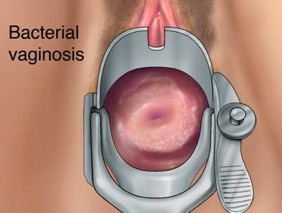
Wet Prep Interpretation
The learner should:
- Proceed as for vaginal culture collection and obtain a sample of vaginal fluid
- On a single glass slide, place a drop of NaCl and a drop of KOH
- Mix a small amount of vaginal fluid with each solution and apply coverslip
- Immediately after preparation, take the prepared slide to the microscope and use low magnification (10x) to focus
- Look for clue cells, white cells and trichomonads on the NaCl field, and for budding hyphae on the KOH field
- Perform a whiff test and, if available, check for pH
- Discuss findings and treatment with supervising clinician and patient
NOTE: This entire module is also available in PDF Format.
Learning Outcomes
The learning objectives of cervical cytology collection are to:
- Demonstrate understanding of the background, technique and interpretation of traditional slide and liquid-based cervical cytology
- Demonstrate the appropriate technique in collecting cervical cytology
- Describe the screening intervals in different age groups
- Counsel patients appropriately about the role of cervical cytology in the detection of cervical cancer and dysplasia
- Communicate with the patient in a respectful, sensitive manner during the examination
The cervical cytology screening visit is also an opportunity to address and counsel patients on various additional issues. The collection of cervical/vaginal material for cultures and wet prep is generally done for a specific indication, such as vaginitis or for screening for sexually transmitted infections. Various vaginal conditions, including vulvovaginal candidiasis, bacterial vaginosis, trichomoniasis and leukocytosis, can be visualized on wet prep.
Best Practices
We found that most learners are introduced to these basic skills during clinical skills courses. In some instances, opportunities to perform these skills on gynecologic exam instructors or standardized patients would follow. There is currently a dearth of simulation type or web-based opportunities to practice these skills outside the clinical arena. Most learners gain the majority of opportunities to perform the skills during their clinical clerkship in the form of supervised clinical contact.
An informal survey of 17 medical schools around the country confirmed these findings. We provide the following materials to help standardize the instruction and evaluation process in a manner consistent with the best practices of academic institutions across the country.
Therefore, we suggest introducing instruction of cytology, cervical culture collection and wet prep as a simulation using a pelvic model and prepared slides of wet prep findings, and then supplementing clinical experience during the obstetrics and gynecology clerkship with standardized patient experience.
Case Scenario
Below is a simple case scenario that can be used for a standardized patient station.
Miss Jones is a 22-year-old woman coming to the clinic for a routine gynecological examination. She has never had a pelvic exam.
The learner’s tasks are to:
- Obtain a focused history
- Perform a relevant physical examination and cervical cytology/culture specimen collection
- Discuss initial diagnostic impression and workup/follow up plan with the patient
Checklist
Checklists may be used for teaching and/or for assessment. Grading may be by yes/no or expanded to include assessment of task completion to fully/partially/not done/not applicable.
The checklist should be completed by a trained observer with knowledge of the proper technique of the clinical skill. Due to the nature of the techniques required, an in-room observer is the essential to evaluate the technical skills. This observer may be a health care professional or GTA. If the session is taped, the history and communication portion of the checklist may be completed by a trained remote observer.
Instructions for the Cervical Cytology, Cultures Station
This station is 20 minutes in length. Please use this time to interview the patient and perform a focused physical exam.
Please note that learners are expected to obtain a focused history, family history, social history and medications, and to collect a cervical cytology and cervical cultures. Make sure you discuss with the patient your initial diagnostic impression and work-up and follow-up plan.
Once learners leave the examination room, you may not re-enter. You are expected to complete their note and give it to the staff when finished. This is a 20-minute station; the staff member will knock on the door when five minutes remain and at the end of the session.
| Done | Not Done |
|
| General Approach and Communication Skills | ||
| Properly introduced themselves to the patient | ||
| Asked patient how they would like to be addressed | ||
| Clarified purpose of visit | ||
| Washed hands or used an antiseptic wash | ||
| Used appropriate draping techniques for patient privacy | ||
| Maintained sterile technique | ||
| Performed the exam in a systematic fashion | ||
| Prefaced exam maneuvers with simple explanations | ||
| Established and maintained rapport with the patient | ||
| Made the patient feel comfortable | ||
| Closed the exam in an appropriate manner | ||
| Focused History | ||
| LMP | ||
| Age at first menses | ||
| Duration of flow | ||
| Days between periods | ||
| History of abnormal pap test | ||
| History of sexually transmitted infections | ||
| Sexual activity, men/women/both | ||
| Number of partners | ||
| Age at first intercourse | ||
| Type of contraception | ||
| Cervical Cytology Collection | ||
| Selected appropriately sized speculum and warmed it | ||
| Inserted the speculum correctly and visualized the cervix | ||
| Collected the cervical cells correctly using spatula and cytobrush | ||
| Used correct technique to collect cells into the vial | ||
| Labeled the specimen appropriately | ||
| Cervical Culture | ||
| Used the appropriate collection vial for the specimen | ||
| For a cervical culture, placed the swab in the endocervix for 10 seconds | ||
| Capped off and labeled specimen appropriately |
Performance Assessment
The cervical cytology and cervical/vaginal culture collection skills are best assessed through direct observation of either a clinical encounter, a standardized patient encounter or simulated session using a pelvic model. The wet prep collection and interpretation skills are best assessed using vaginal fluid, if available, or other similar material (such as hand lotion). If the latter is used, the student should have access to prepared slides demonstrating the findings commonly seen on a wet prep, such as clue cells, white cells, trichomonads or hyphae.
The preceding checklist can be used for performance assessment of a clinical encounter for cervical cytology and cervical culture collection.
Practical Tips
We suggest that the cervical cytology, cultures and wet prep skills examination be introduced to students during the first two years of medical school in the form of didactics, practice on models and a gynecological teaching associate (GTA). This exercise should be repeated with an GTA during the clinical years, if feasible, to supplement the student’s clinical experience. The performance assessment should occur as part of an objective structured clinical examination at end of the obstetrics and gynecology clerkship or at the end of the third year.
Resources
- American Society for Colposcopy and Cervical Pathology
- Saslow, Soloman, Lawson et al JLGTD, March 2014, 2012 (online)
- Saslow, Soloman, Lawson et al. CA: Cancer J Clin, 2012 May-June: 62(3):147-172.
Susan Bliss, MD

