ASSOCIATION OF PROFESSORS OF GYNECOLOGY AND OBSTETRICS

Breast Exam
- Back to Module Listing
- Description
- Learning Outcomes
- Best Practices
- Checklist
- Performance Assessment
- Practical Tips
- Resources
Description
General Approach/Interpersonal Communication Skills
Learners should introduce themselves to the patient, confirm the patient’s identity and establish how they want to be addressed. Learners should wash their hands with soap and warm water or alcohol-based antiseptic. Learners should inform the patient that they are performing a breast exam. This is a good time to ask the patient if they have noticed any lumps or other problems with their breasts. Learners should be organized and have the patient properly draped, i.e. cover areas not being examined.
Inspection
Asking the patient to lower the gown, learners should visually inspect the breasts from front and sides. Learners should look for size, symmetry (some variation is normal), shape, contour (flattening, masses and dimpling), skin (color, edema, rashes, thickening and venous pattern) and scars (previous surgery andinjuries). Learners should do the inspection with the patient performing arm maneuvers: overhead (#1), waist (#2), and leaning forward (#3). Learners are looking for any retraction when the patient is leaning forward, or contracting the pectoral muscles.

#1 #2 #3
Palpation
- Lymph nodes
- Cervical nodes: These nodes are found along the sides of the neck.
- Axillary nodes: The patient is in a seated position using appropriate draping technique. With patient’s arm at their side and the examiner lifting the arm away from side to access nodes (#4).
- Supraclavicular nodes: These nodes are found along a line immediately above the clavicle. This is done by learners stepping around behind the patient.
#4
- Bimanual palpation while patient sitting
- Learners should perform bimanual palpation with the patient in a seated position, using appropriate draping technique.
- Learners should use the right hand above/left hand below to palpate the right breast. Learners should use the pads of the fingertips to compress the breast tissue between fingertips. Using this technique, learners can check for consistency, nodules, masses and tenderness, which might not be felt in supine breast exam. Repeat for left side by standing on patients’ left side and reversing hands (left on top, right on bottom).
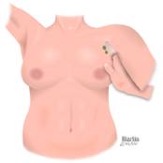
- Complete breasts palpation while patient is supine
- Learners should pull out the footrest and ask the patient to put their arm overhead during supine palpation. The arm overhead helps to stretch the breast tissue against the chest wall.
- Learners should then perform a complete palpation of the breasts. Learners should use the flat part of the fingers (and a rotary motion) against the chest wall using a radial or spiral pattern without missing areas, compressing the breast tissue against the chest wall in all quadrants of the breast (#5). Learners should be noting tissue consistency, elasticity, nodules, indurations, masses and tenderness.

#5
- Learners should palpate all of the breast, which continues up the chest wall to the clavicle (collar bone) and towards the axilla (armpit).
- Learners should inspect and palpate the nipples (#6), looking for size, shape, inversion, rashes, ulceration, discharge, scaling, crusting, elasticity, retraction, areolar edema and masses. Learners should gently grasp and compress the nipple and areolar tissue between thumb and index finger, noting the color consistency and quantity of any discharge (#7).

#6 #7
Copyright 2008 Association of Professors of Gynecology & Obstetrics
NOTE: This entire module is also available in PDF Format.
Learning Outcomes
There are differing recommendations regarding the use of the clinical breast exam (CBE). The American College of Obstetricians and Gynecologists (ACOG) recommends a clinical breast exam every year for women aged 19 years and older. The American Cancer Society (ACS) and United States Preventive Services Task Force (USPSTF) agree that there is insufficient evidence to assess the benefits and harms of clinical breast exam. The ACS goes further and does not recommend routine clinical breast exams. All organizations agree that all women should be familiar with how their breasts normally look and feel, and report changes to their health care provider.
The CBE may be used in clinical scenarios to complement mammography. Additionally, a CBE can serve as an opportunity for women and their health care provider to discuss changes in their breasts, early detection testing and factors in the woman’s history that might make her more likely to develop breast cancer.
The purpose of teaching the medical student how to perform the clinical breast exam is to:
- Practice detecting a lump or change in the appearance of the breast that may indicate breast disease.
- Practice evaluating other breast conditions that may require medical attention, such as mastitis.
- Practice appropriate communication skills when performing a sensitive exam, such as the breast examination, on patients.
Best Practices
Evidence suggests that simulation training can help learners achieve proficiency and increased confidence in performing clinical breast exams1,2. The addition of an intimate examination assistant or standardized patient may have an additional positive performance on learners as well3. A comprehensive literature review has shown that learners utilizing standardized patients perform better than learners taught by faculty (as assessed by a clinical examination). Learners utilizing silicone models have higher sensitivity for detecting breast lumps (as assessed by ability to detect lumps in silicone breast models4).
Therefore, we recommend that standardized patients be used to teach the clinical breast examination to learners, in combination with practicing on silicone models.
Case Scenario
Ms. Smith is a 52-year-old female who came to the clinic today because she noticed a breast lump while taking a shower last week.
Vital signs: BP 135/80 P 70/min R 14/min Temp 99.5°F (37.5°C)
Learner tasks are to:
- Obtain a focused history
- Perform a relevant physical examination
- Discuss initial diagnostic impression and workup plan with the patient
Checklist
Checklists may be used for teaching and/or for assessment. The checklist should be completed by a trained observer with knowledge of the proper technique of the breast examination. Due to the nature of the techniques required, an in-room observer is the minimum essential. In addition, the checklist may be completed by a trained remote (video) observer (useful for assessment of communication and interpersonal skills while the in-room observer focuses on technical skills) and/or the patient or model/GTA.
| Done | Not Done | |
| Properly introduces themselves to the patient | ||
| Establishes and maintains rapport with the patient | ||
| Washes hands or used an antiseptic wash | ||
| Uses appropriate draping techniques | ||
| Performs the exam in an organized fashion | ||
| Makes the patient feel comfortable | ||
| Uses appropriate non-verbal skills | ||
| Closes the exam in an appropriate manner | ||
| With patient sitting, inspects both breasts from front and sides | ||
| Asks patient to put arms overhead | ||
| Asks patient to put arms on her waist and press elbows forward | ||
| Asks patient to lean forward with arms out in front | ||
| With patient sitting, palpates the cervical, supraclavicular and axillary lymph node | ||
| With patient sitting, performs bimanual palpation of the breast | ||
| Performs complete palpation of the breast with the flat part of the fingers | ||
| Performs palpation of the axillary tail | ||
| Gently palpates and expresses nipples (only if pt c/o nipple discharge) |
Performance Assessment
Breast examination skills are best assessed through direct observation or a standardized patient exercise. The checklist can be used for performance assessment. The case scenario above can be used for a standardized patient station.
Practical Tips
We suggest that the breast examination be introduced to the learners during the first two years of medical school in the form of didactics, practice on models and a standardized patient (SP) exercise. The SP exercise may be repeated during the clinical years. The performance assessment may occur as part of an objective structured clinical examination at the end of the obstetrics and gynecology clerkship or at the end of the third year.
Resources
- Pugh, C. M. and L. H. Salud. “Fear of missing a lesion: use of simulated breast models to decrease student anxiety when learning clinical breast examinations.” Am J Surg 2007; 193(6): 766-770.
- Naylor, R. A., et al. “Can medical students achieve skills proficiency through simulation training?” Am J Surg 2009; 198(2): 277-282.
- Hendrickx, K., et al. “Learning intimate examinations with simulated patients: the evaluation of medical students’ performance.” Med Teach 2009; 31(4): e139-147.
- Gaffan J, Dacre J, Jones A. Educating undergraduate medical learners about oncology: a literature review. J Clin Oncol 2006; 24(12):1932-9.
- U.S. Preventive Services Task Force: http://www.uspreventiveservicestaskforce.org
- American College of Obstetricians and Gynecologists: http://www.acog.org
- American Cancer Society: http://www.cancer.org
- Bates’ Guide to Physical Examination & History Taking. Eleventh Edition. By Lynn S. Bickley, Peter Szilagyi. Chapter 10; The Breasts and Axillae.
Sarah Page-Ramsey, MD

